Scientists from Koa Health and Birmingham and Solihull Mental Health NHS Foundation Trust developed a machine learning model that uses electronic health records to detect the risk of a mental health crisis in patients over 28 days.
The machine-learning algorithm continuously monitors patients for the possibility of a mental health crisis using anonymized electronic health records. Moreover, half of the crises were properly predicted 28 days ahead of time by the model, with a low false-positive rate.
The opportune identification of patients who are at risk of mental health distress can prompt ameliorated results and the alleviation of burdens and expenses.
In any case, the high commonness of mental health issues implies that the manual review of intricate patient records to prepare proactive care decisions isn’t plausible in practice.
Subsequently, the scientists developed a machine learning model that utilizes electronic health records to continuously monitor patients for risk of mental health distress over 28 days.
The model accomplishes an area under the receiver operating characteristic curve of 0.797 and an area under the precision-recall curve of 0.159, prognosticating distress with a sensitivity of 58% at a specificity of 85%.
A follow-up half-year prospective study assessed their algorithm’s utilization in clinical practice and noticed predictions to be clinically significant as far as either managing caseloads or alleviating the risk of crisis in 64% of cases.
To the extent of the scientists’ knowledge, this study is the first to ceaselessly predict the risk of a wide range of mental health distress and to investigate the additional value of such predictions in clinical practice.
Identification of Patients at the Risk of a Mental Health Distress
Almost 1 billion individuals globally live with a mental disorder. With the worldwide mental health crisis significantly exacerbated by the COVID-19 pandemic of 2019, healthcare systems face an increasing demand for mental health services combined with a lack of skilled personnel.
In clinical practice, unique demand emerges from mental health crises — circumstances in which patients can neither care for themselves nor work effectively and circumstances in which patients might hurt themselves or others.
Opportune treatment can forestall worsening the symptoms that lead to such crises and ensuing hospitalization. Be that as it may, patients are now and again already experiencing mental health distress when they access urgent care pathways as their primary entry point to a medical clinic or psychiatric facility.
By this point, it is beyond any good time to apply preventative strategies, restricting the capability of psychiatric services to allocate their restricted assets early appropriately. In this way, identifying patients at risk of experiencing a crisis before its occurrence is vital to working on patient results and managing caseloads.
Tools that can Serve as a Utility in Mental Health Sector
Working as an NHS psychiatrist, I saw too many people arrive in our services through the Accident and Emergency Department. By the time we saw them, they were usually very sick, and had often experienced problems with their relationships, finances, employment and housing. Putting the pieces back together was almost always expensive, time-consuming, and painful for the people involved. We were delighted to be chosen as a Wave 1 NHS Test Bed to partner with Birmingham and Solihull NHS Mental Health Foundation Trust. We shared a vision of moving from reactive care – driven by crisis – to proactive care – driven by prediction and prevention. We have delivered outstanding results in this trial and look forward to continuing the development work. We believe this is the future of mental healthcare in the UK and worldwide.
Dr. Oliver Harrison, CEO Koa Health
In occupied clinical settings, the manual review of huge quantities of information across numerous patients to make proactive care decisions is impractical, unsustainable, and prone to error.
Consequently, shifting such tasks to the computerized analysis of electronic health records (EHRs) holds an extraordinary guarantee to reform health services by empowering large-scale ceaseless data review.
Research has previously shown the feasibility of predicting critical events related to a broad scope of healthcare issues, including hypertension, diabetes, circulatory failure, hospital readmission, and in-hospital death.
Nonetheless, the mental health literature is restricted to predicting explicit kinds of events —for example, suicide, self-harm, and first-episode psychosis — as opposed to ceaselessly expecting the broadness of psychological health crises that require critical care or hospitalization.
Many parts remain unknown about the feasibility of questioning machine learning models consistently to assess the risk of an unavoidable mental health crisis.
This would empower optimizing healthcare staff allocation and forestalling crisis onset. Moreover, even a profoundly exact predictive model doesn’t ensure further improved mental health results or long-term cost savings; accordingly, it stays unclear whether new predictive technologies could give tools that are helpful to mental health service practitioners.
Studying Model Performance for Different Mental Health Issues
In this research, the feasibility of predicting any mental health crisis event is investigated, no matter what its cause or the underlying mental disorder, and the scientists scrutinize whether such predictions can offer an added benefit to clinical practice.
Prevention is widely seen as the holy grail of treating mental health problems. Using AI to predict mental health crises can enable timely and proactive instead of reactive interventions to mitigate or prevent mental health crises and truly help both patients and healthcare systems. We were so excited when the results from the clinical implementation of our model suggested that our predictions may have indeed prevented more serious symptoms. Providing the right intervention at the right time sits at the core of Koa’s approach.
Dr. Aleksandar Matic, Koa Health’s R&D Director
The supporting presumption would be that historical patterns predict future psychological health crises and that such patterns can be identified in real-world EHR information, regardless of its meager condition, noise, errors, and systematic bias.
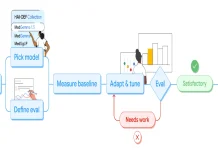
To this end, the scientists developed a mental crisis risk model by contributing EHR information gathered in over more than seven years (2012-2018) from 17,122 patients into a machine learning algorithm.
The researchers assessed how precisely the model ceaselessly predicted the risk of a psychological health crisis in the following 28 days from an arbitrary moment, with the end goal of supporting dynamic care decisions in clinical practice.
The researchers also examined how the model’s performance differentiated across a scope of mental health disorders, various ethnic, age, and gender groups, and variations in information availability.
Besides, they conducted a forthcoming cohort study to assess the crisis prediction algorithms in clinical practice from 26 November 2018 to 12 May 2019.
The crisis predictions were followed through on a bi-weekly premise by four distinct groups of clinicians (altogether, 60 clinicians going to 1,011 cases over more than a half year), who assessed whether and how such predictions assisted them with managing caseload needs and alleviating the risk of crisis.
The Endpoint
The machine learning methodologies which are trained on historical patient records have exhibited the extensive potential to predict critical events in various clinical areas (for instance, circulatory failure, diabetes, cardiovascular disorders, and more).
In the mental health sector, the prediction algorithms have ordinarily centered around the detection of individual propensity to die by self-harm/suicide or develop psychosis, with no extant investigations attempting to constantly identify significant psychological health events or those that would require readmission for urgent care or hospitalization.
In any case, a few studies have considered predictions of spontaneous clinic readmissions no matter what their supporting reason and got AUROCs somewhere in the range of 0.750 and 0.791 for the prediction of the risk of readmission in no less than 30 days (like the scientists’ results of 0.797 in 28 days or less).
Albeit such algorithms can significantly help medical services, their capability to improve caseload management or forestall undesirable health results is restricted by:
- The query timing (just at discharge instead of ceaselessly) and
- The nature of readmissions (not explicit for any disorder in particular; most such readmissions are not preventable).
Running predictions continuously gives an updated risk score in light of the most recently available information, which ordinarily contains the most predictive data, which is, on account of mental health, vital to further developing healthcare management and results.
The increasing demand for mental healthcare is progressively provoking hospitals to effectively work on the identification of novel strategies for anticipating demand and better deploying their restricted assets to improve patient results and diminishing long-term costs.
Assessing technological plausibility and clinical value are basic strides before the integration of prediction models into routine care models.
According to this viewpoint, the scientists’ study prepares for better resource optimization in the mental health services domain and empowers the long-anticipated shift in the psychological health paradigm from reactive care to preventative care.
Article Source: Garriga, R., Mas, J., Abraha, S. et al. Machine learning model to predict mental health crises from electronic health records. Nat Med (2022). https://doi.org/10.1038/s41591-022-01811-5
https://www.koahealth.com/blog-post/groundbreaking-machine-learning-algorithm-accurately-predicts-mental-health-crises-/
Learn More:
Top Bioinformatics Books ↗
Learn more to get deeper insights into the field of bioinformatics.
Top Free Online Bioinformatics Courses ↗
Freely available courses to learn each and every aspect of bioinformatics.
Latest Bioinformatics Breakthroughs ↗
Stay updated with the latest discoveries in the field of bioinformatics.
Tanveen Kaur is a consulting intern at CBIRT, currently, she's pursuing post-graduation in Biotechnology from Shoolini University, Himachal Pradesh. Her interests primarily lay in researching the new advancements in the world of biotechnology and bioinformatics, having a dream of being one of the best researchers.