T cells are a category of immune cells. They play an important role in maintaining normal bodily functions and battling diseases. When faced with antigens, naive T cells undergo specific changes and develop into different types of cells with distinct properties, abilities, and functions. This process is controlled by genetic as well as molecular factors. T cells are of four types, CD4+, CD8+, γδ, and natural killer T (NKT) cells. These cells fight against various infections, chronic diseases, cancers, and autoimmune diseases. Scientists from Xi’an Jiaotong University review the current understanding of T cells, emphasizing the features, development pathways, regulatory mechanisms, contributions of exhausted CD8+ T cells in fighting against tumors, the supportive role of CD4+ T cells in boosting CD8+ T cell responses, and potential applications of T cells in therapies.
What are T-cells?
T cells mediate cell-based immunity against foreign substances called antigens. They prevent diseases and keep us healthy. T cells develop in the thymus from thymocyte progenitors. Thymocyte progenitors are derived from bone marrow. Among the four types of T cells, the major ones are CD4+ and CD8+. They are commonly called αβ T cells. αβ T cells have T Cell Receptors (TCR) on them. These receptors recognize the antigens presented by MHC molecules on antigen-presenting cells (APCs). MHC stands for Major Histocompatibility Complex. Then, naive αβ T cells get activated and differentiate into CD4+ helper cells or CD8+ cytotoxic cells. The helper cells and cytotoxic cells kill infected cells, regulate the immune system, and provide long-term protection. A small portion of T cells become memory cells, which can rapidly respond and protect the body upon encountering the same pathogens again. Parallelly, there exists a small subpopulation of CD4+ T cells called regulatory T (Treg) cells, which maintain peripheral immune tolerance.
The knowledge of T cells has increased significantly over the past few decades. Therefore, novel strategies making use of T-cell functions have been developed considerably and have even shown remarkable clinical efficacy.
From Naive to Mighty: The Journey of Immune Cell Development
T cell development occurs in the thymus, starting with thymocyte progenitors from the bone marrow. It involves stages of double negative (DN), double positive (DP), and single positive (SP) cells. The DN stage does not contain CD4 and CD8 surface markers, while the DP stage contains both CD4 and CD8 markers. The SP stage consists of either CD4+ or CD8+ cells. DN thymocytes are categorized into DN1 to DN4 stages based on CD44 and CD25 expression (CD44 and CD25 are cell surface markers or antigens used to identify different populations of immune cells). In the DN2a stage, T-cell lineage commitment (determination of the fate of T cells as either αβ T cells or γδ T cells) occurs through a process called Notch Signaling. The actual differentiation of T cells into αβ or γδ T cells occurs at the DN2b and DN3a stages. In the DN3 cells, a functional pre-T cell receptor (pre-TCR) complex is formed, leading to the development of CD4+CD8– immature single positive (ISP) and DP cells. Once T cells express a TCRβ chain, they can initiate rearrangement of the TCRα chain and subsequently develop a fully functional αβTCR on their surface. This αβTCR is capable of recognizing complexes formed by MHC I or MHC II molecules presenting peptide antigens, which are displayed by antigen-presenting cells (APCs) in the thymus. Then, TCR signaling and cytokine stimulation drive the CD4/CD8 lineage choice. The key transcription factors that determine CD4+ or CD8+ T cell development are Thpok and Runx3. Thpok is the primary regulator for CD4 lineage commitment, while Runx3 facilitates CD8+ T cell development, and the balance between Thpok and Runx3 determines the lineage choice between CD4+ and CD8+ T cells.
How T Cells Defend the Body Against Acute Infection and Inflammation
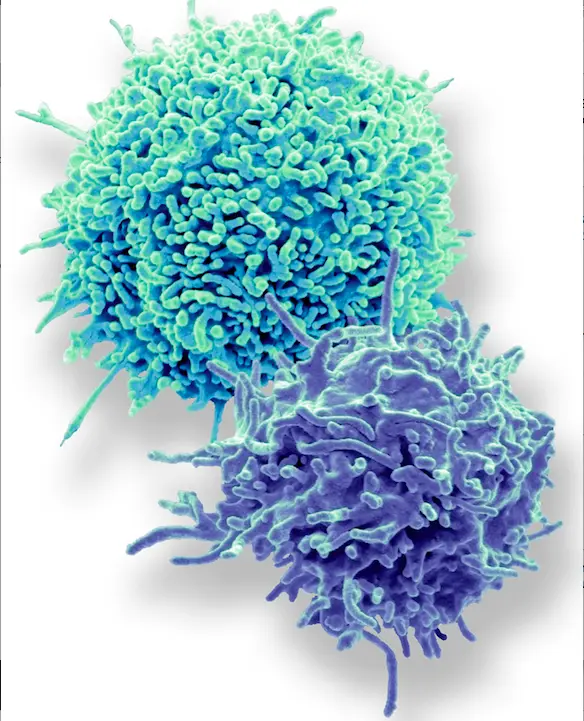
The CD8+ and CD4+ T cells fight against acute infections and inflammation caused by microbial pathogens. CD8+ T cells, also known as cytotoxic T cells, are the main responders to viral infections and participate in the defense against bacterial and protozoal pathogens. CD8+ T cells differentiate into effector CD8+ cells and memory CD8+ cells. Effector CD8+ T cells secrete pro-inflammatory cytokines to inhibit viral replication. They also express various chemokines to attract other inflammatory cells to the sites of infection. Effector CD8+ T cells are responsible for eliminating pathogens and providing immediate protection, while memory CD8+ T cells provide long-term immune protection by forming a memory of the pathogen.
CD4+ T cells, also called helper T cells, have four sub-types, and each of the sub-types has a unique role in the immune response. The Th1 subset is crucial for protective immunity against intracellular pathogens, like viruses and bacteria. Th2 cells are involved in humoral immune reactions against extracellular parasites and allergic inflammation, while Th17 cells produce pro-inflammatory cytokines and are elicited in infections by bacterial and viral microorganisms. Th22 cells protect against infections locally on mucosal tissues and skin. CD4+ T cells also indirectly contribute to pathogen control by regulating the functions of other immune cells. They activate pro-inflammatory macrophages, enhancing their antimicrobial effectiveness. They are also important for memory CD8+ T cell generation and their heightened response to subsequent antigen encounters.
The Dynamism of T Cells: Fighting Chronic Infections and Cancer
In the case of chronic infections and cancer, the antigen stimulation is continuous, hence, T cells adopt a unique trajectory of differentiation called exhaustion. Exhausted T cells (Tex) have been found in chronic viral infections such as HIV (Human Immunodeficiency Virus) and almost every mouse and human cancer. In such chronic conditions, the discovery of stem-like progenitor CD8+ Tex (Tpex) cells has opened new doors for the development of next-generation cancer immunotherapies.
Exhausted CD8+ cells are a subset of cytotoxic T lymphocytes (CTLs) that have become dysfunctional or “exhausted” due to persistent antigen stimulation in chronic infections and cancer. Exhausted CD8+ cells exhibit functional impairments, including decreased cytokine production, reduced cytotoxicity, and compromised proliferative ability. Exhausted CD8+ T cells can be reinvigorated through immune checkpoint blockade (ICB), which involves the use of antibodies that block inhibitory receptors like PD-1 (programmed cell death protein 1) or CTLA-4 (cytotoxic T-lymphocyte-associated protein 4). These reinvigorated cells regain their effector functions and proliferative capacity, allowing them to control chronic infections or tumors better.
Stem-like progenitor CD8+ Tex cells represent a specific subset of Tex cells that possess characteristics similar to stem cells. The stem cell-like properties of these cells include self-renewal and differentiation potential. They have been associated with responsiveness to ICB. Reinvigorating these cells through checkpoint blockade can restore their effector functions and enhance anti-tumor responses. Hence, ICB can serve as one of the most promising clinical cancer therapies.
Even CD4+ cells enhance the anti-tumor response of CD8+ CTLs through various means. They do so by helping the CD8+ T cells during their priming (initial activation and preparation for the immune response), promoting clonal expansion and effector function, enhancing migration and tissue infiltration, supporting memory formation, and transmitting help signals (interactions between different immune cells that facilitate the optimal functioning of the immune response) through costimulatory and cytokine signals.
Rethinking Disease Prevention: T Cell Based Immunotherapy
These days, T cells have found applications in immunotherapy approaches. Such approaches are called T cell-based immunotherapies. They are used to treat diseases such as cancer and autoimmune disorders. In the case of cancer, three main techniques have been developed that show promising clinical efficacy:
- Immune Checkpoint Blockade (ICB): uses monoclonal antibodies to block immune checkpoint molecules or inhibitory receptors to enhance the anti-tumor immune response.
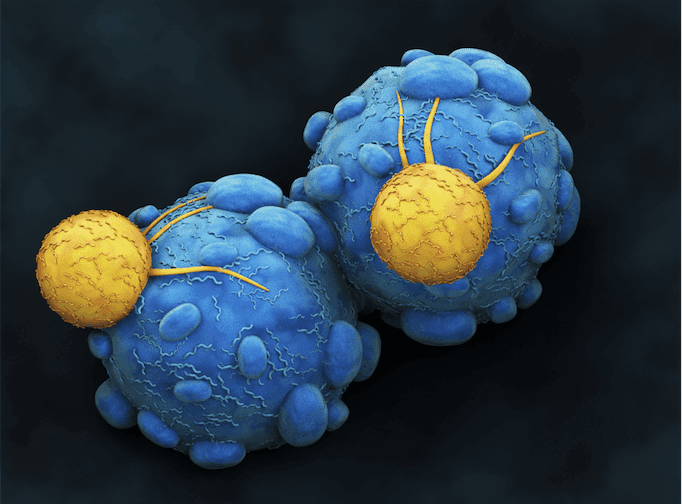
- Bispecific T cell Engagers (TCEs): are artificially created monoclonal antibodies with two binding sites. One binds to T cells and the other to a tumor-specific antigen, forming a link between them. The T cell induces an immune response, and the cancer cells get killed.
- Adoptive Cell Therapy (ACT): this method involves collecting the patient’s T cells and modifying them genetically to enhance cancer cell recognition and destruction. The cells are transferred back into the patient’s body.
Autoimmune disorders are caused when immune cells attack the host’s healthy cells. Traditionally, they are treated with therapeutic drugs, but immunotherapy for autoimmune disorders is gaining significance. CAR-T (Chimeric Antigen Receptor T-cell) therapy has the potential to treat autoimmune diseases. One strategy in this method is the application of CAR-T cells expressing the peptide Major Histocompatibility Complex (pMHC). It can interact with and eliminate autoreactive T cells. A variant of CAR-T is CAR-Treg, which utilizes the immunosuppressive activity of Treg cells. This method has not only shown clinical efficacy in various autoimmune diseases but has also demonstrated immunosuppression of effector T cells in organ transplants in pre-clinical models.
Conclusion
The current understanding of the T-cell involves its development, its types, and its functions in carrying out immune responses to acute and chronic diseases. The rise in T-cell based immunotherapies shows a promising future for people suffering from chronic and autoimmune diseases. However, the scope is still limited, as the focus is currently only on classical T-cell populations. Therefore, further exploration and research are required to better tap the potential of T cells in therapeutic strategies.
Article Source: Reference Paper
Learn More:
Neegar is a consulting scientific content writing intern at CBIRT. She's a final-year student pursuing a B.Tech in Biotechnology at Odisha University of Technology and Research. Neegar's enthusiasm is sparked by the dynamic and interdisciplinary aspects of bioinformatics. She possesses a remarkable ability to elucidate intricate concepts using accessible language. Consequently, she aspires to amalgamate her proficiency in bioinformatics with her passion for writing, aiming to convey pioneering breakthroughs and innovations in the field of bioinformatics in a comprehensible manner to a wide audience.