Researchers at University College London discovered multimorbidity and comorbidity illness trends using a dataset spanning 3.8 million patients in England. Patients and clinicians can use the study findings and interactive online tools to prevent and detect comorbid conditions. In contrast, biomedical researchers and pharmaceutical manufacturers can use them to provide lead compounds targeting common or sequential disease pathways and instruct clinical trial design.
Multimorbidity is a condition in which patients have two or more chronic illnesses. Hypertension, depression/anxiety, and chronic pain are thought to be more common than other conditions. Millions of individuals live with multimorbidity as they age, and the proportion of persons afflicted in this fashion is anticipated to climb in the coming decades. On the other hand, medical education and training, healthcare delivery, clinical guidelines, and research have evolved to focus on a single disease at a time.
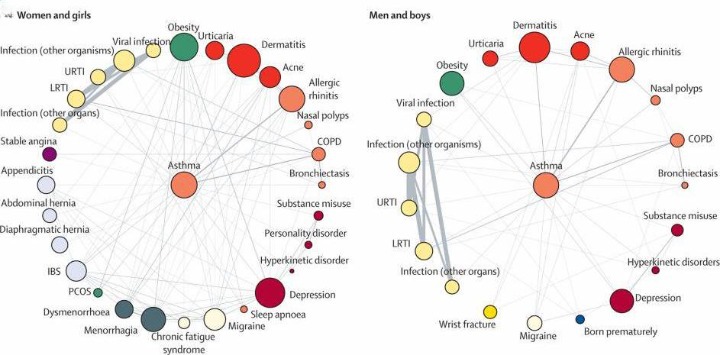
The study has pinpointed the contrasts in multimorbidity and comorbidity patterns by age, gender, and ethnicity using data from nearly 4 million English National Health Service patients, with implications for clinical practice, drug development, and research on the disease pathways.
The team used routine health record data to rigorously discover patterns of clustering among 308 common mental and physical health disorders in men and women across all ages and ethnicities in the new study published in the Lancet Digital Health. The authors have also provided online tools for others to explore these patterns in greater depth.
Major Findings From The Multimorbidity Analysis
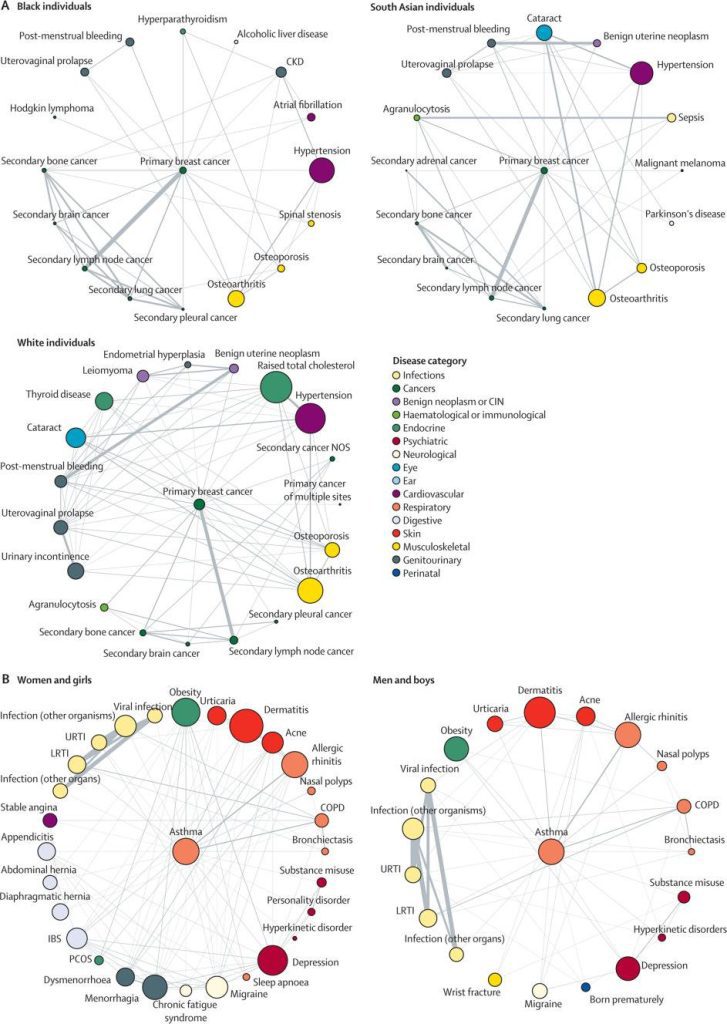
Image Source: https://doi.org/10.1016/S2589-7500(22)00187-X
The study found that the percentage of people with two or more reported conditions was higher in Caucasian people than in Black and South Asian people. Heart failure frequently co-occurs with hypertension, osteoarthritis, stable angina, myocardial infarction, renal disease, type II diabetes, and chronic obstructive pulmonary disease (COPD), among other things. Hypertension was most strongly related to renal diseases in people aged 20 to 29. Still, it was also connected with dyslipidemia (Exceptionally high levels of cholesterol in the blood), obesity, and type II diabetes in people aged 40 and over.
Breast cancer was linked to a variety of comorbidities such as Atrial fibrillation (irregular heart rhythm affecting proper blood flow to the heart) and Parkinson’s in people of different races, asthma to a variety of comorbidities in both sexes, and bipolar illness to an array of comorbidities in younger people. In younger patients (aged 20-29 years), bipolar affective disorder was associated with higher total cholesterol, liver failure, and obesity, whereas renal diseases and thyroid disease were common in older individuals with this illness (aged 70–79 years).
According to the researchers, these findings provide data and resources to improve health, care, and planning for people with more than one ailment. Co-author and Professor Aroon Hingorani from the UCL Institute of Cardiovascular Science says that the information obtained from minority groups and younger people has frequently been omitted from other studies focusing on multimorbidity analysis. But, this study has given a more inclusive and representative perspective on multimorbidity by using electronic health data. This is one area in which the NHS electronic health records and data science can provide valuable insights.
Way Forward
According to Professor Spiros Denaxas from the UCL Institute of Health Informatics, millions of people suffer from numerous diseases, but our understanding of how and when these occur is restricted. This study endeavor is the first step toward understanding how these diseases interact and determining the best way to treat them.
Future research should investigate the pandemic’s impact on multimorbidity patterns. Typically, biomedical research focuses on discrete disorders, with little attention paid to overlapping pathogenic pathways; therefore, the non-random connections discovered in this study or by the users of our online tools could provide the groundwork for further research into shared disease processes and risk factors. In genetic association studies, overlapping genetic loci for different phenotypes suggest that any given therapeutic target could increase the risk of many illnesses. Researchers could investigate non-pharmacological therapies for risk factors that affect non-random multimorbidities. Furthermore, studies determining whether comorbidities are induced by the unfavorable effects of therapeutic medications or procedures could provide patients and physicians with critical information for weighing the benefits and risks of various treatment options.
Article Source: Reference Paper | Reference Article | Data Availability
Learn More:
Top Bioinformatics Books ↗
Learn more to get deeper insights into the field of bioinformatics.
Top Free Online Bioinformatics Courses ↗
Freely available courses to learn each and every aspect of bioinformatics.
Latest Bioinformatics Breakthroughs ↗
Stay updated with the latest discoveries in the field of bioinformatics.
Shwetha is a consulting scientific content writing intern at CBIRT. She has completed her Master’s in biotechnology at the Indian Institute of Technology, Hyderabad, with nearly two years of research experience in cellular biology and cell signaling. She is passionate about science communication, cancer biology, and everything that strikes her curiosity!